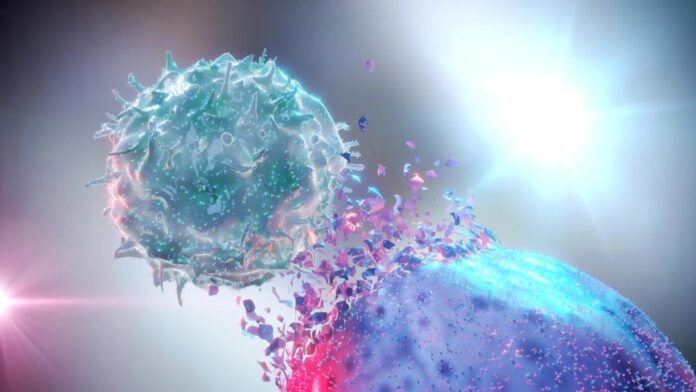
A new study published in Nature Cancer reveals that combining radiation therapy with immunotherapy can dramatically improve treatment outcomes for lung cancer patients, even those whose tumors are resistant to immunotherapy alone. Researchers at Johns Hopkins University, in collaboration with the Netherlands Cancer Institute, have identified the molecular mechanisms behind this effect, known as the abscopal effect, where radiation triggers a systemic immune response against cancer cells throughout the body.
Зміст
The Challenge of Immunotherapy Resistance
Immunotherapy harnesses the patient’s own immune system to fight cancer, but many tumors remain unresponsive. This is often due to “cold” tumors – those lacking key immune markers like high mutation rates or PD-L1 expression. These tumors don’t initially attract immune attention, making them difficult to target. The research team sought to understand why this resistance occurs and how to overcome it.
How Radiation “Warms Up” Cold Tumors
The study analyzed blood and tumor samples from 72 lung cancer patients undergoing either immunotherapy alone or radiation followed by immunotherapy. Using advanced genomic and immunological techniques, the team discovered that radiation therapy can transform “cold” tumors into “warm” ones by triggering inflammation and attracting immune cells, including T cells.
The abscopal effect was directly observed: radiation at the primary tumor site induced an immune response that attacked distant, untreated cancer cells. Patients whose tumors exhibited this “warming up” effect had significantly better outcomes than those who did not receive radiation therapy.
“Our findings highlight how radiation can bolster the systemic anti-tumor immune response in lung cancers unlikely to respond to immunotherapy alone,” stated lead study author Justin Huang.
The Molecular Mechanisms at Play
Researchers found that radiation causes tumors to release molecules that alert the immune system. This, in turn, activates T cells that recognize and attack cancer cells based on their unique genetic mutations. By confirming this effect in laboratory tests, the team demonstrated that radiation-primed T cells effectively target cancer cells carrying specific mutation-associated neoantigens.
Implications for Future Treatment
These results suggest that radiation therapy could be strategically combined with immunotherapy to overcome resistance in a wider range of cancer patients. Further research is underway to identify biomarkers that predict which patients will benefit most from this combination approach. The study also highlights the importance of international collaboration in advancing cancer treatment, as evidenced by the partnership between Johns Hopkins and the Netherlands Cancer Institute.
The findings demonstrate that radiation therapy isn’t just a local treatment, but a systemic immune modulator with the potential to unlock new therapeutic avenues for previously untreatable cancers.